Glaucoma is one of the leading causes of irreversible blindness worldwide. Yet, it often goes unnoticed until significant damage has occurred. Regular eye tests are essential tools in identifying and managing this condition effectively. In this article, we will explore the importance of glaucoma screenings, what to expect during these tests, and strategies for living with glaucoma.
Understanding Glaucoma: A Brief Overview
Elaucoma eye test refers to a group of eye diseases that result in damage to the optic nerve, often caused by abnormally high pressure in the eye. Understanding the nature of glaucoma is crucial for prevention and timely intervention.
What is Glaucoma?
Glaucoma is a progressive condition that leads to vision loss if left untreated. The disease can be categorized primarily into two types: open-angle glaucoma and angle-closure glaucoma. It often presents without noticeable symptoms, making regular screenings vital for early detection. As the disease progresses, individuals may experience a gradual loss of peripheral vision, which can go unnoticed until significant damage has occurred. This is why awareness and education about glaucoma are essential, especially for those at higher risk.
Types of Glaucoma
There are several types of glaucoma, each with distinct characteristics:
Open-Angle Glaucoma: This is the most common form, where the eye’s drainage canals become clogged over time, leading to increased intraocular pressure (IOP). It typically develops slowly and can be managed effectively with medication or surgery if caught early.
Angle-Closure Glaucoma: This type occurs when the iris bulges forward, blocking the drainage angle, causing a rapid rise in IOP and often resulting in acute symptoms such as severe eye pain, headache, nausea, and vomiting. This form of glaucoma is considered a medical emergency and requires immediate treatment to prevent permanent vision loss.
Normal-Tension Glaucoma: In this rare type, optic nerve damage occurs even though IOP is within the normal range. It is characterized by progressive damage to the optic nerve, and its exact cause remains unclear, making it a challenging condition to diagnose and manage.
Congenital Glaucoma: This form occurs in infants and is caused by abnormal eye development. It often requires prompt surgical treatment to prevent irreversible damage to the optic nerve and vision.
In addition to these primary types, there are also secondary glaucomas, which can develop as a result of other medical conditions or eye injuries. For instance, conditions like diabetes or high blood pressure can increase the risk of developing secondary glaucoma. Furthermore, certain medications, particularly corticosteroids, have been linked to elevated IOP, making it essential for patients to discuss their medication history with their eye care professionals. Understanding these nuances can empower individuals to take proactive steps in monitoring their eye health.

The Importance of Regular Eye Tests
Regular eye tests play a critical role in identifying glaucoma before significant damage occurs. Early detection through screening can save eyesight and improve quality of life. Below, we explore how these tests help in managing the disease.
Detecting Glaucoma Early
Detection of glaucoma in its early stages is essential for effective management. Eye tests measure various factors such as IOP, visual field, and optic nerve health. These assessments help identify individuals at risk and allow for timely intervention.
Many people may not experience symptoms until they reach advanced stages of glaucoma; therefore, regular screening becomes a lifesaver. Eye care professionals can initiate treatment early and prevent progression to irreversible blindness.
In addition to standard tests, advancements in technology have introduced innovative methods for early detection. Optical coherence tomography (OCT) provides high-resolution images of the optic nerve, allowing for a more detailed examination of its structure. This technology can detect subtle changes that may indicate the onset of glaucoma, even before traditional methods can. As a result, patients can benefit from a more comprehensive evaluation, leading to more personalized and effective treatment strategies. Read more about detecting glaucoma at https://www.health.harvard.edu/topics/glaucoma
Monitoring Glaucoma Progression
For those already diagnosed with glaucoma, regular screenings serve as a means of monitoring disease progression. Eye tests can reveal changes in vision and eye pressure, which can inform adjustments to treatment plans.
Continual assessment allows eye care professionals to determine the effectiveness of medications or other therapies and adapt them as necessary. This proactive approach is crucial for maintaining eye health in patients with glaucoma.
Furthermore, the role of patient education cannot be overstated in the management of glaucoma. Understanding the nature of the disease, its risk factors, and the importance of adherence to treatment regimens empowers patients to take an active role in their eye health. Educational programs and resources provided by eye care professionals can help demystify the condition, enabling patients to recognize the importance of regular check-ups and to report any changes in their vision promptly. This collaborative approach between patients and healthcare providers is vital for optimizing outcomes and preserving vision over the long term.
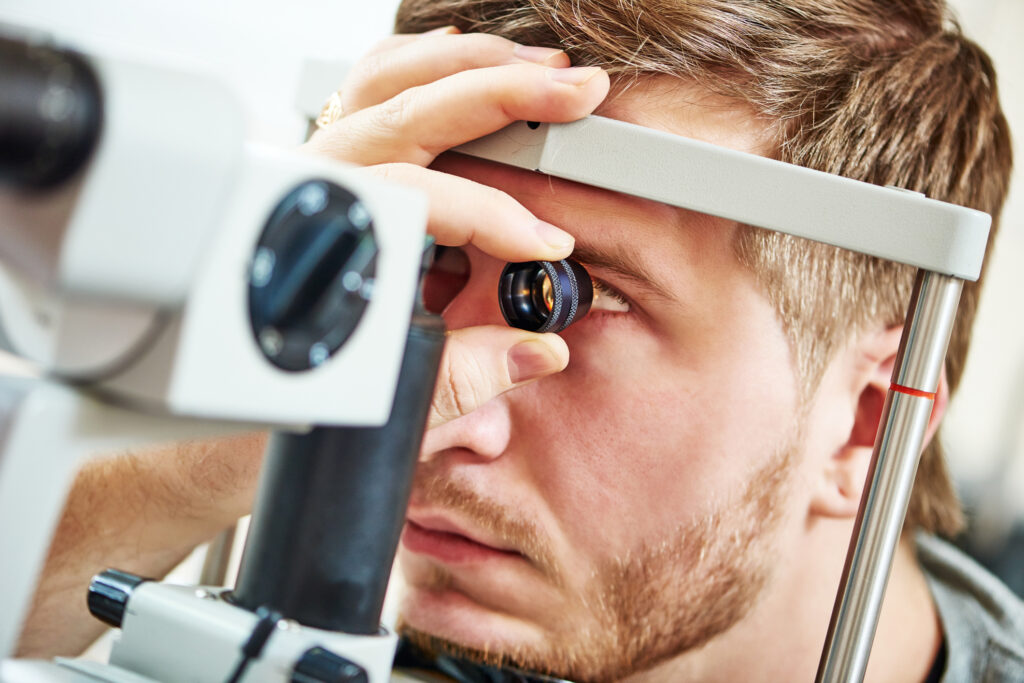
The Eye Test for Glaucoma
Understanding what to expect during an eye test for glaucoma can alleviate anxiety for patients. These tests are generally straightforward, and knowing the process can make visits less daunting.
What to Expect During the Test
The eye test for glaucoma usually begins with a comprehensive eye exam conducted by an optometrist or ophthalmologist. Key components include:
Tonometry: This test measures intraocular pressure. It may involve the use of a puff of air or a small probe.
Visual Field Test: This assesses peripheral vision and helps identify any loss of sight that may indicate glaucoma damage.
Ophthalmoscopy: An exam that allows the doctor to view the optic nerve directly and check for signs of damage.
The entire process may take around an hour, and many tests are non-invasive, involving little discomfort. Patients are often encouraged to ask questions during the examination, as this can help demystify the procedures and foster a collaborative atmosphere between the patient and the healthcare provider. It’s also helpful to arrive with a list of any symptoms or concerns, as this can guide the discussion and ensure that all relevant issues are addressed.
Understanding Your Test Results
Test results will be discussed during your visit, typically including measurements of IOP and observations about the optic nerve. Normal IOP ranges from 10 to 21 mm Hg, and deviations may warrant further investigation. The healthcare provider may also explain how factors such as age, family history, and ethnicity can influence glaucoma risk, providing a broader context for your individual results.
Additionally, visual field test results help indicate whether there is any functional loss in vision, guiding treatment decisions. It is essential to understand these results and engage in discussions with your healthcare provider regarding any concerns. Patients may also be advised on lifestyle changes or preventive measures that can help manage eye health, such as regular exercise, maintaining a healthy diet rich in antioxidants, and adhering to prescribed medications. This proactive approach not only aids in the management of glaucoma but also empowers patients to take an active role in their eye health journey. To Learn more interpreting test results click here.
Frequency of Glaucoma Screenings
Determining how often you should have glaucoma screenings can depend on various factors, including age, family history, and previous eye health issues. Generally, the following guidelines are recommended:
Recommended Screening Intervals
For most adults, it is advisable to have comprehensive eye exams every two years. However, if you fall into a higher risk category, more frequent screenings may be necessary:
Individuals over 40 years of age should have their eyes tested every one to two years.
Those with a family history of glaucoma, diabetes, or high eye pressure may need annual screenings.
At-risk populations, including individuals with certain medical conditions or eye injuries, should consult with their healthcare provider regarding appropriate testing intervals.
Factors Affecting Screening Frequency
Various personal factors can influence how often an individual should be screened for glaucoma. Besides family history and age, these factors include:
Ethnicity: Certain racial and ethnic groups, such as African Americans and Hispanics, are at a higher risk for glaucoma.
Medical History: Pre-existing conditions like diabetes or hypertension can elevate risk.
Eye Conditions: Previous eye injuries or surgeries can lead to increased susceptibility to glaucoma.
In addition to these factors, lifestyle choices can also play a significant role in eye health. For instance, regular physical activity and a balanced diet rich in antioxidants may help maintain optimal eye pressure and overall ocular health. Engaging in activities that promote cardiovascular health can improve blood flow to the eyes, potentially reducing the risk of developing glaucoma. Furthermore, avoiding smoking and managing stress levels are crucial, as these factors can adversely affect eye health over time.
It’s also important to note that glaucoma often develops without noticeable symptoms until significant damage has occurred. This makes regular screenings even more critical, as early detection can lead to more effective management and treatment options. Many eye care professionals utilize advanced diagnostic technologies, such as optical coherence tomography (OCT) and visual field testing, to assess the health of the optic nerve and detect any early signs of glaucoma. Staying proactive about your eye health can make a substantial difference in preserving vision and preventing complications associated with this silent disease.
Living with Glaucoma
Receiving a diagnosis of glaucoma can be overwhelming, but there are ways to manage the condition effectively. Understanding treatment options and lifestyle modifications can significantly enhance the quality of life for individuals living with glaucoma.
Managing Glaucoma Symptoms
While glaucoma may not have overt symptoms until it progresses, individuals can manage the condition through various strategies. Regular follow-up appointments are crucial for tracking changes and ensuring appropriate treatments are adjusted as needed.
In addition to medication compliance, patients are encouraged to be vigilant about their symptoms. Aspects such as frequent headaches, halos around lights, or sudden vision changes warrant immediate consultation with an eye care professional.
Treatment Options for Glaucoma
Treatment for glaucoma typically revolves around lowering intraocular pressure to prevent further damage to the optic nerve. Common options include:
Medications: Eye drops are the most common treatment and may include beta-blockers, prostaglandin analogs, and carbonic anhydrase inhibitors.
Laser Therapy: Procedures such as laser trabeculoplasty may be recommended to improve drainage and decrease IOP.
Surgery: In advanced cases, surgical intervention may be necessary to create a new drainage canal or reduce the formation of aqueous humor.
Living with glaucoma requires ongoing vigilance, but with appropriate care and regular screenings, individuals can maintain their vision and quality of life.
In conclusion, regular eye tests for glaucoma are vital for early detection, monitoring progression, and managing the condition effectively. As we have discussed, understanding the nature of glaucoma, the testing processes, and the implications of test results can empower patients to take an active role in their eye health. It is essential to adhere to recommended screening schedules and to communicate openly with eye care professionals to maintain optimal vision for years to come.
Related : Glaucoma Causes and Symptoms: Early Detection for Better Outcomes

